A Decade of Surgery Problems Plague Rhode Island Hospital
Monday, June 11, 2018
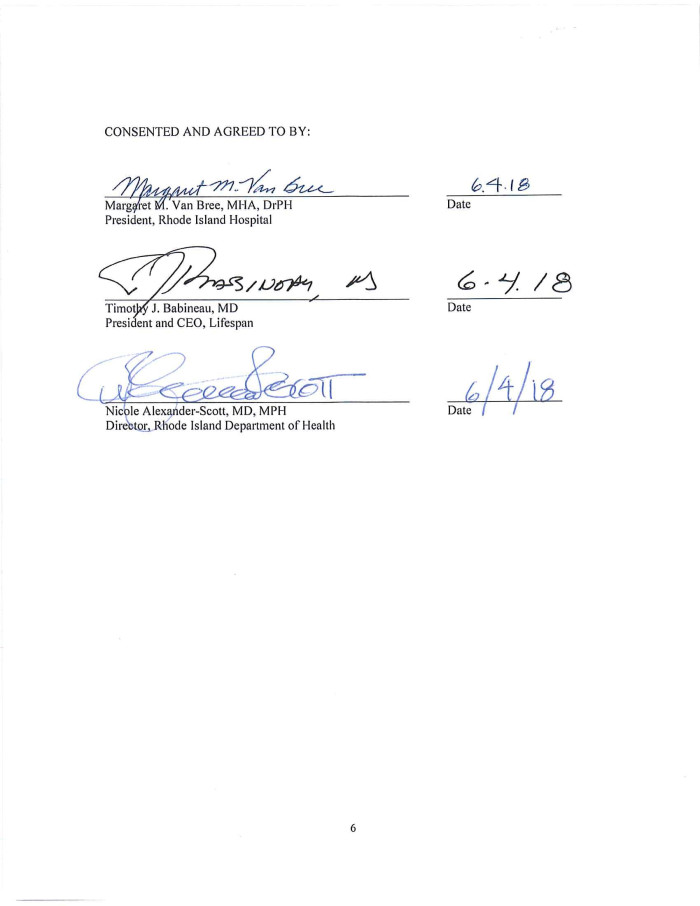
Friday’s announcement of a consent agreement between Rhode Island Hospital and the Rhode Island Department of Health (DOH) is just the most recent enforcement action against the hospital over the past decade.
RI Hospital has been hit repeatedly now by State regulators for conducting wrong side and wrong person surgeries. In addition, Rhode Island Hospital has been embroiled in multiple lawsuits including a number of cases of major litigation. Just in the past three years, juries hit the hospital with nearly $90 million in judgments in just two cases.
On Friday, the agreement set forth a series of regulatory actions including the requirement that RI Hospital spends $1 million in new training requirements.
GET THE LATEST BREAKING NEWS HERE -- SIGN UP FOR GOLOCAL FREE DAILY EBLAST“Whenever preventable errors occur in hospital settings, it is essential that we scrutinize those errors carefully and that facilities make the systems changes needed to ensure that they do not occur again. Rhode Island is home to some of the preeminent healthcare facilities in the region and the country. Inspections and regulatory work by the Department of Health are critical to ensuring that our hospitals maintain that status, and to ensuring that the healthcare system as a whole continues to provide quality patient care,” said Director of Health Nicole Alexander-Scott, MD, MPH.
READ THE FULL CONSENT DECREE BELOW
According to this most recent enforcement action, RIH failed to implement and sustain processes and systems to provide care and services in accordance with its w1itten policies and procedures pertaining to patient identification and verification, verification of procedure site/side, and provider's orders for diagnostic services in the following cases:
1. On 2/21/2018, Patient ID #2 underwent a computed tomography angiography of the brain and neck intended for another patient.
2. On 2/26/2018, Patient ID #1 was not c01Tectly identified and as a result underwent an angiogram intended for another patient.
3. On 3/12/2018, Patient ID #3 unde1went a surgical ve1tebroplasty on Patient ID
#3's C-6 which was intended to be done on C-7.
4. On 3/16/2018, Patient ID #8 underwent a mammogram of the right breast intended for another patient.
Rhode Island Hospitals miscues are not unique in healthcare. “Analyzing medical death rate data over an eight-year period, Johns Hopkins patient safety experts have calculated that more than 250,000 deaths per year are due to medical error in the U.S. Their figure, published May 3 in The BMJ, surpasses the U.S. Centers for Disease Control and Prevention’s (CDC’s) third leading cause of death — respiratory disease, which kills close to 150,000 people per year,” writes Johns Hopkins Medicine.
Record Judgments Against RI Hospital
Just a year ago, a $61 million judgment following a $40 million jury verdict in the eight-day trial in Providence Superior Court was awarded. As of September 2017, when this verdict was returned, it is the largest medical malpractice verdict in Rhode Island history. The patient had had his right leg amputated, after he developed severe blood clots as a result of the doctors’ failure to place him on a blood thinner. The jury found that errors made by multiple physicians and physicians-in-training led to the injury. Sfameni v. Rhode Island Hospital, according to the law firm Decof Decof and Barry.
In 2015, a jury has delivered a $25.6 million verdict against Rhode Island Hospital in what was then the largest negligence verdict ever in Rhode Island.
Rhode Island Hospital acknowledged that several doctors and nurses were negligent in caring for an Exeter man who went there in 2009 after hitting his head, and who left with permanent, debilitating injuries.
The hospital acknowledged before trial that its staff misdiagnosed Carl Beauchamp, failed to check on him and missed signs that his condition was worsening.
The jury on awarded Beauchamp $15 million for pain and suffering and $5.6 million for medical expenses. His wife was awarded an additional $5 million.
Previous Enforcement Action by Department of Health
In October of 2010, GoLocal reported that Rhode Island Hospital was hit with a $300,000 fine by the Rhode Island Department of Health for an August 4th incident when, during neurosurgery, a small piece of a drill bit broke off and was left lodged in a patient's scalp.
The Department of Health conducted a joint investigation with the Center for Medicare & Medicaid Services (CMS) and discovered that the hospital is not actively ensuring that the operating room staff is following existing hospital policy. RIH’s surgical count policy states that if a surgical tool or device is unaccounted for at the end of surgery, an x-ray of the patient should be done before the patient leaves the operating room to assure that the tool or device is not inside the patient. In the previous August incident, no x-ray was taken and the surgical count was documented as correct.
“We found evidence they were not following their policies once again,” said Dr. David Gifford, Director of the Department of Health, “and the staff was reporting issues in the operating room that weren’t addressed.” Gifford added that operating room staff reported the anesthesiologist neglected to wear a mask during administration as well. “It’s a continued pattern of non-compliance with their own policies and procedures,” added Gifford.
According to Modern Healthcare, Rhode Island Hospital, was fined $150,000 in 2009 and was ordered to put video cameras in all its operating suites and must undergo surgery procedure protocol observation for at least one year in response to another wrong-site surgery that took place at the hospital.
“The hospital's continued failure to effectively implement policies and practices to ameliorate this particular problem is frustrating and significantly damages the public's perception of safety and the credibility of R.I. Hospital's ability to consistently provide for safe surgical procedures,” wrote David Gifford, director of health for the Rhode Island Health Department, in a letter to the hospital's chief executive.
Modern Healthcare reported, “The incident marks the fifth wrong-site surgery that has occurred at 632-bed Rhode Island Hospital since 2007. The most recent occurrence involved a wrong-site finger surgery, according to health department documents. Three previous procedures were wrong-site head surgeries.”
Then-Rhode Island Hospital President and CEO Timothy Babineau said in a written statement that his hospital remains “committed to decreasing the frequency of medical errors including wrong-site surgeries.”
Today, Babineau is the Chief Executive Officer of Lifespan — RI Hospitals’ parent company.
Other Major Fines
In 2012, RI Hospital was forced to pay $5.3 million in penalties. The Hospital reimbursed federal health care programs approximately $2.6 million dollars and paid the federal government approximately $2.7 million in double and triple damages for ordering medically unnecessary overnight patient hospital stays and then submitting claims for payment to federally funded Medicare and Medicaid programs.
An investigation by the United States Attorney’s Office for the District of Rhode Island; Office of Inspector General of the U.S Department of Health and Human Services (OIG-HHS); and the Federal Bureau of Investigation determined that during the period from January 1, 2004, through December 31, 2009, medically unnecessary overnight hospital admissions were ordered for approximately 260 patients who underwent stereotactic radiosurgery, otherwise known as Gamma Knife treatment. The investigation also revealed that Rhode Island Hospital’s claims for reimbursement for the overnight admissions to Medicare and Medicaid falsely represented that the admissions were medically necessary when, in fact, they were not.
Related Slideshow: RI Dept. of Health, RI Hospital Consent Agreement - June 2018
Related Articles
- Researchers at RI Hospital Discover Trend Among Veterans Fatally Overdosing
- NEW: NIH Awards RI Hospital $5.8 Million to Support Cancer Research Program
- Nurses Union to Picket in Front of RI Hospital on July 9
- NEW: RI Hospital Says Nurse Picket Thursday Will Not Interrupt Services
- See the List: RI Hospitals and Surgeons with Highest Complication Rates
- Women & Infants Becomes First RI Hospital with Leapfrog Distinction
- RI Hospitals’ Emergency Times Among Worst in US
- RI Hospital to Utilize Google Glass in Innovative New Study
- RI Hospital: Legalizing Med. Marijuana Does Not Increase Youth Use
- Are RI Hospitals Ready for an Ebola Outbreak?
- RI Hospitals With the Highest Complication Rates
- RI Hospital Nurses and Technicians Reject Contract Offer From Lifespan
- RI Hospitals: How Big and How Much Revenue
- RI Hospital Files Obstetrics Application With State—Likely to Trigger Calls for Payment to Prov
- RI Hospital Awarded $5.8 Million Grant for Skeletal Health
- Tuesday on LIVE: Prof. Lawless, Former RI Hospital President Iannuccilli, & The Horse-Eyed Men
- LIVE: Ripple Effect - RI Hospital’s Chief of Trauma Dr. Adams On Impact of Impaired Driving Crashes
- NEW: RI Hospital Refused to Divulge Name of Employee Accused Sexual Assault
- RI Hospitals’ Emergency Room Waiting Times - Big Differences
- NEW: RI Hospital Nurses Ratify New Three Year Contract with Lifespan
- RI Hospital Earns National Award For Excellence in Cancer Care
- RI Hospitality Names Award Winners
- Brown University & RI Hospital Earn Grants to Teach Addiction Screening